Cephalosporins Drugs
Cephalosporins are beta-lactam antimicrobials used to manage a wide range of infections from gram-positive and gram-negative bacteria. The five generations of cephalosporins are useful against skin infection, resistant bacteria, meningitis, and other infections. This activity describes the indications, contraindication, and possible adverse effects of cephalosporins and will highlight the mechanism of action, adverse event profile, monitoring, route of administration, as well as other key factors.
Cephalosporins can be taken orally or injected into a vein (intravenous injection), depending on the infection.
Cephalosporins are grouped together based on the type of bacteria that they’re most effective against. These groups are referred to as generations. There are five generations of cephalosporins.
To understand the differences between the generations, it’s important to understand the difference between Gram-positive and Gram-negative bacteria.
One of the main distinctions between the two is their cell wall structure:
- Gram-positive bacteria have thicker membranes that are easier to penetrate. Think of their cell wall as a chunky, loose-knit sweater.
- Gram-negative bacteria have thinner membranes that are harder to penetrate, making them more resistant to some antibiotics. Think of their wall as a piece of fine chain mail.
Cephalosporins are a type of antibiotic used to treat a range of bacterial infections. There are different generations of cephalosporins, and some are better suited to treat certain infections than others.
If you have to take antibiotics, make sure to tell your doctor about all other medications you take, as well as any previous allergic reactions to antibiotics.
Cephalosporins are a slightly modified chemical “twin” to penicillins due to their beta-lactam chemical structure. (See Figure for a comparison of the beta-lactam ring structure, spectrum of activity, and route of administration across different classes of medications.) Because of these similarities, some patients who have allergies to penicillins may experience cross-sensitivity to cephalosporins.
Indications: Cephalosporins are used to treat skin and skin-structure infections, bone infections, genitourinary infections, otitis media, and community-acquired respiratory tract infections.
Mechanism of Action: Cephalosporins are typically bactericidal and are similar to penicillin in their action within the cell wall. Cephalosporins are sometimes grouped into “generations” by their antimicrobial properties. The 1st-generation drugs are effective mainly against gram-positive organisms. Higher generations generally have expanded spectra against aerobic gram-negative bacilli. The 5th-generation cephalosporins are active against methicillin-resistant Staphylococcus aureus (MRSA) or other complicated infections.
Specific Administration Considerations: Patients who are allergic to penicillins may also be allergic to cephalosporins. Patients who consume cephalosporins while drinking alcoholic beverages may experience disulfiram-like reactions including severe headache, flushing, nausea, vomiting, etc. Additionally, like penicillins, cephalosporins may interfere with coagulability and increase a patient’s risk of bleeding. Cephalosporin dosing may require adjustment for patients experiencing renal impairment. Blood urea nitrogen (BUN) and creatinine should be monitored carefully to identify signs of nephrotoxicity.
Patient Teaching & Education: Patients who are prescribed cephalosporins should be specifically cautioned about a disulfiram reaction, which can occur when alcohol is ingested while taking the medication. Additionally, individuals should be instructed to monitor for rash and signs of superinfection (such as black, furry overgrowth on tongue; vaginal itching or discharge; loose or foul-smelling stool) and report to the prescribing provider.
It is also important to note that cephalosporin can enter breastmilk and may alter bowel flora of the infant. Thus, use during breastfeeding is often discouraged.
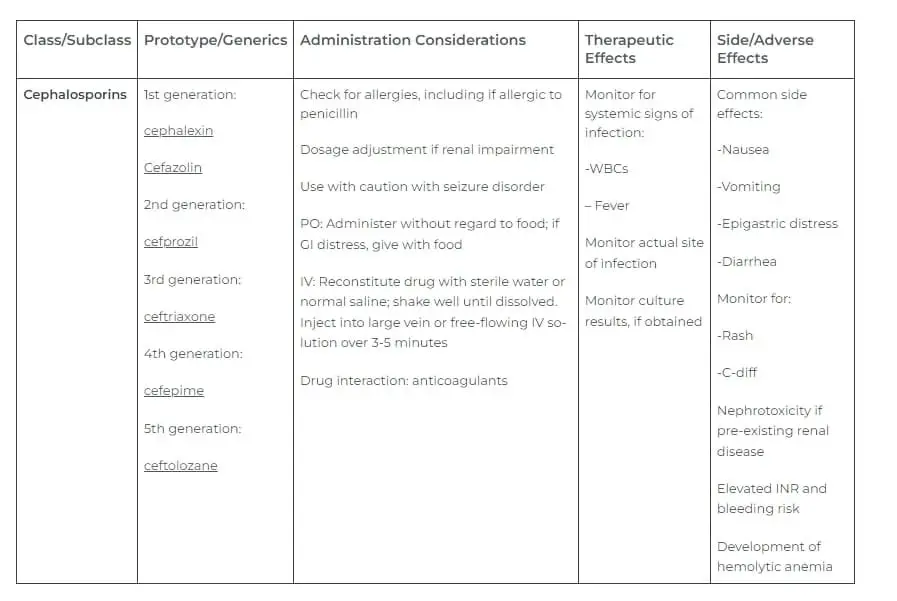
cephalosporins are antimicrobials grouped into five generations based on their spectrum of coverage against gram-positive and gram-negative bacteria and their temporal discovery.
First-generation cephalosporins have coverage against most gram-positive cocci as well as some gram-negative bacteria, e.g., Escherichia coli (E. coli), Proteus mirabilis, and Klebsiella pneumonia.
Second-generation cephalosporins have coverage against Haemophilus influenza (H. influenza), Moraxella catarrhalis, and Bacteroides spp.
Third-generation cephalosporins have less coverage against most gram-positive organisms but have increase coverage against Enterobacteriaceae, Neisseria spp., and H. influenza.
Fourth-generation cephalosporins have similar coverage as third-generation cephalosporins but with additional coverage against gram-negative bacteria with antimicrobial resistance, e.g., beta-lactamase.
Fifth-generation cephalosporins have coverage against methicillin-resistant staphylococci and penicillin-resistant pneumococci.
First-generation cephalosporins
First-generation cephalosporins are very effective against Gram-positive bacteria. But they’re only somewhat effective against Gram-negative bacteria.
First-generation cephalosporins might be used to treat:
- skin and soft tissue infections
- UTIS
- strep throat
- ear infections
- pneumonia
Some first-generation cephalosporins are used as prophylactic antibiotics for surgery involving the chest, abdomen, or pelvis.
Examples of first-generation cephalosporins include:
- Cephalexin
- Cefadroxil
- Cephradine
SUMMARY
First-generation cephalosporins are more effective against Gram-positive bacteria, though they also work against some Gram-negative bacteria.
Second-generation cephalosporins
Second-generation cephalosporins also target some types of Gram-positive and Gram-negative bacteria. But they’re less effective against certain Gram-positive bacteria than first-generation cephalosporins are.
They’re often used to treat respiratory infections, such as bronchitis or pneumonia.
Other infections sometimes treated with second-generation cephalosporins include:
- Ear infections
- Sinus infections
- UTIs
- Gonorrhea
- Meningitis
- sepsis
Examples of second-generation cephalosporins include:
- Cefaclor
- Cefuroxime
- Cefprozil
SUMMARYSecond-generation cephalosporins target both Gram-positive and Gram-negative bacteria. But they’re a little less effective against Gram-positive bacteria compared to first-generation cephalosporins
Third-generation cephalosporins
Third-generation cephalosporins are more effective against Gram-negative bacteria compared to both the first and second generations. They’re also more active against bacteria that may be resistant to previous generations of cephalosporins.
The third generation also tend to be less active than previous generations against Gram-positive bacteria, including Streptococcus and Staphylococcus species.
One third-generation cephalosporin, ceftazidime (Fortaz), is often used to treat Pseudomonas infections, including hot tub folliculitis.
Third-generation cephalosporins may also be used to treat:
- Skin and soft tissue infections
- Pneumonia
- UTIs
- Gonorrhea
- Meningitis
- Lyme disease
- Sepsis
A few examples of third-generation cephalosporins include:
- Cefixime
- Ceftibuten
- Cefpodoxime
SUMMARYThird-generation cephalosporins are effective against many Gram-negative bacteria and bacteria that haven’t responded to first- or second-generation cephalosporins.
Fourth-generation cephalosporins
Cefepime is the only fourth-generation cephalosporin that’s available in the United States. While effective against a variety of Gram-positive and Gram-negative bacteria, it’s usually reserved for more severe infections.
Cefepime can be used to treat the following types of infections:
- Skin and soft tissue infections
- Pneumonia
- UTIs
- Abdominal infections
- Meningitis
- Sepsis
Cefepime can be administered intravenously or with an intramuscular injection. It may also be given to people with a low white blood cell count, which can increase the risk of developing a severe infection.
SUMMARYFourth-generation cephalosporins work against both Gram-positive and Gram-negative bacteria. They’re generally used for more severe infections or for those with weakened immune systems.
Fifth-generation cephalosporins
You may hear fifth-generation cephalosporins referred to as advanced-generation cephalosporins. There’s one fifth-generation cephalosporin, ceftaroline (Teflaro), available in the United States.
This cephalosporin can be used to treat bacteria, including resistant Staphylococcus aureus (MRSA) and Streptococcus species, that are resistant to penicillin antibiotics.
Otherwise, ceftaroline’s activity is similar to that of third-generation cephalosporins, although it isn’t effective against Pseudomonas aeruginosa.
SUMMARYCeftaroline is the only fifth-generation cephalosporin available in the United States. It’s often used to treat infections, including MRSA infections, that are resistant to other antibiotics.
As with any kind of medication, you can be allergic to cephalosporins. The most common sign of an allergic reaction to cephalosporins is a skin rash.
In rare cases, cephalosporins may cause a serious allergic reaction known as anaphylaxis.
Symptoms of anaphylaxis include:
- hives
- flushed skin
- swollen tongue and throat
- breathing difficulties
- low blood pressure
- rapid or weak pulse
- nausea or vomiting
- diarrhea
- dizziness
- fainting
GET HELPAnaphylaxis can be life-threatening. Seek immediate medical treatment if you’re taking a cephalosporin and experience symptoms of anaphylaxis.
Cephalosporins can cause a range of side effects, including:
- stomach upset
- nausea
- vomiting
- diarrhea
- yeast infection or oral thrush
- dizziness
One of the more serious side effects that can occur is a C. difficile infection. This infection typically occurs after a long course of antibiotics and can be potentially life-threatening.
Symptoms to watch out for include:
- watery diarrhea
- abdominal pain
- fever
- nausea
- decreased appetite
You can help to prevent stomach upset and diarrhea by:
- taking probiotics, which can help to add good bacteria to your digestive tract
- following the instructions that come with your medication, as some antibiotics should be taken with food, while others should be taken on an empty stomach
- avoiding foods that can contribute to stomach upset, such as spicy or greasy foods
Cephalosporins are generally safe for most people, including those who are pregnant. In fact, some first-generation cephalosporins are commonly used to treat UTIs in pregnant people.
However, you shouldn’t take cephalosporins if you’re breastfeeding.
Cephalosporins can sometimes interact with other medications you’re taking. Make sure to tell your healthcare provider about all other medications you take, including supplements, vitamins, and over-the-counter medications.
Mechanism of Action
Bacteria synthesize a cell wall that is strengthened by cross-linking peptidoglycan units via penicillin-binding proteins (PBP, peptidoglycan transpeptidase). The beta-lactam rings bind to the penicillin-binding protein and inhibit its normal activity. Unable to synthesize a cell wall, the bacteria die.
Staphylococcus aureus that is initially susceptible to cephalosporins, can develop resistance by changing the structure of the penicillin-binding proteins. S. aureus does this by having a gene that encodes a modified penicillin-binding protein; this prevents the cephalosporin’s beta-lactam rings from inactivating the protein. The bacterium that develops this mechanism of resistance is called methicillin-resistant Staphylococcus aureus (MRSA). As indicated above, out of the five generations of cephalosporin, only the fifth generation ceftaroline has coverage against methicillin-resistant Staphylococcus aureus. Another crucial resistance mechanism is producing the enzyme beta-lactamase, which cleaves the beta-lactam ring, preventing it from attaching to the penicillin-binding proteins, e.g., peptidoglycan transpeptidase. Beta-lactamase inhibitors can be co-formulated with cephalosporins to increase their spectrum of activity, e.g., ceftazidime/avibactam and ceftolozane/tazobactam.
Administration
First-generation: Cefazolin, cephalothin, and cephapirin are administered parenterally.
The administration route for cefadroxil and cephalexin is oral.
Cephradine administration can be parenteral or oral.
Second-generation: Cefuroxime can be administered parenterally or orally. Cefprozil administration is oral. Cefmetazole, cefotetan, and cefoxitin are administered parenterally.
Third-generation: Cefotaxime, ceftazidime, and ceftriaxone administration is via the parenteral route. Cefdinir, cefixime, and cefpodoxime are administered orally. A single intramuscular shot of 125 or 250 mg of ceftriaxone effectively treats uncomplicated gonococcal infection or its complications such as pelvic inflammatory disease or epididymo-orchitis.
Fourth-generation: Cefepime is administered parenterally.
Fifth-generation: Ceftaroline is administered parenterally.
Many of the parenterally administered cephalosporins have short half-lives and need to be given more frequently in patients with normal renal function. Cefazolin and ceftriaxone have a longer half-life; thus, they do not need to be dosed as often. Ceftriaxone is the only cephalosporin that does not need to have its dose modified in the presence of renal failure. However, in patients with both renal and hepatic impairment, the recommended daily dose should not exceed 2 g.
Adverse Effects
Cephalosporins have low toxicity and are generally safe. The most common adverse reactions from cephalosporins are nausea, vomiting, lack of appetite, and abdominal pain.
The less common adverse reaction includes:
Hypersensitivity Reaction
A hypersensitivity reaction to cephalosporin is infrequent and is more common in first and second-generation cephalosporins. Common allergic reaction to cephalosporin includes rash, hives, and swelling. Rarely will the hypersensitivity reaction result in anaphylaxis. Patients who are allergic to penicillin might show a hypersensitive reaction to cephalosporins as well. This cross-reactivity is more common in first and second-generation cephalosporins because they have R-groups more similar to penicillin G. Third generation and beyond show minimal cross-reactivity.
Drug-induce Immune Hemolytic Anemia (DIIHA)
The proposed mechanism of action of DIIHA is that the drug binds to the red blood cell membrane; this causes no harm to the red blood cell itself nor the patient. However, if the patient starts making IgG antibodies against the drug, the antibody will bind the red blood cell. The immune system will react with the abnormal red blood cell resulting in hemolysis. Cefotetan and ceftriaxone are the two cephalosporins most likely to cause DIIHA.
Disulfiram-like Reaction
Cephalosporins containing a methyltetrazolethiol side chain can inhibit the aldehyde dehydrogenase enzyme resulting in the accumulation of acetaldehyde. Cefamandole, cefoperazone, and moxalactam are the most common cephalosporin to present with this reaction.
Vitamin K Deficiency
Certain cephalosporins can inhibit vitamin K epoxide reductase, preventing the production of the reduced(active) vitamin K. Therefore, there is a decreased synthesis of coagulation factors, and the patient is predisposed to hypoprothrombinemia.
Increase Nephrotoxicity of Aminoglycosides
There are reported cases of drug-induced nephrotoxicity when patients take cephalosporin and aminoglycosides in combination, but other factors often cloud the evidence. Therefore, synergistic nephrotoxicity of cephalosporin and aminoglycoside is not to be completely understood.
Pseudomembranous Colitis
Pseudomembranous colitis is often associated with the use of clindamycin and ampicillin. Cephalosporin use is also a common cause of pseudomembranous colitis, especially third-generation cephalosporins.
Contraindications
One of the contraindications of cephalosporin is if patients are allergic to them or those that have had an anaphylactic reaction to penicillin or other beta-lactams antimicrobials.
Ceftriaxone is contraindicated in hyperbilirubinemia neonates because of reports that ceftriaxone displaces bilirubin from albumin, increasing the free bilirubin concentrations and increases the risk of jaundice in neonates. Ceftriaxone reacts to a calcium-containing solution, and it can precipitate in the lungs and kidneys of infants less than 28 days old, which could be life-threatening. Therefore, ceftriaxone is also contraindicated in infants less than 28 days old if they are expected to receive any calcium-containing products.
Monitoring
It is essential to monitor for possible signs of anaphylactic reaction as well as allergic reactions such as hives, itching, and swelling. Physicians and pharmacists also need to monitor renal function periodically because that could potentially warrant a change in the dose and/or dosing frequency of the cephalosporin (except for ceftriaxone).[23] With other possible adverse reactions listed above, monitor CBC for possible signs of drug-induced immune hemolytic anemia or hypoprothrombinemia from vitamin K deficiency. Also, monitor for possible signs of a disulfiram-like reaction or pseudomembranous colitis.
Toxicity
Testing the effects of high dosage cephalosporin in rabbits, there is new evidence of nephrotoxicity due to its effect on the mitochondria system of the kidney. Cefepime overdose can result in seizures and encephalopathy. Studies show it to potentially result from cefepime crossing the blood-brain barrier and displaying concentration-dependent ϒ-aminobutyric acid (GABA) antagonism, which can also occur with toxic doses of penicillin G. Other studies show altered mental statues and a triphasic wave discharge on electroencephalogram (EEG). Discontinuation of cefepime demonstrates normalization of mental status.
Exercise caution with cephalosporin treatment in patients with a history of seizures, especially with poor renal function.
Reference: National Library of Medicine